Innovation and Patient empowerment in healthcare
Patient empowerment
Healthcare professionals spend years becoming experts in how to treat disease to help people. When fast decisions need to be made, they are there and can deliver what is best in that situation to make someone healthy. Traditionally the healthcare workers in primary care, the family physician, district nurse, and others, had time to build up relationships with their community and deliver their expertise in context. They had a greater understanding the patient’s world and made decisions based on both clinical parameters and what the individual was likely to need to not only live, but live well.
In recent years’ restructuring and time-pressures on healthcare systems around the world have reduced the opportunity for long-term physician-patient relationships. More and more decisions are being taken in fast, clinical-focussed settings. For the general public, increased availability of technology and information have given patients the even greater chance to connect, support each other, and access information about their conditions and what they can do to improve their own outcomes. Unless hospitalised, most patients spend more time looking after their health outside clinics than they spend in appointments, and it’s now widely known that patient attitudes, behaviours and actions during self-care time has the power to radically change their health.
These are driving forces behind the evolution of the doctor-patient relationship into one of shared decisions between expert clinicians and informed patients (1). Evidence from recent studies clearly demonstrates that engaging patients in their own care is improves health outcomes, quality of care processes, satisfaction with the care experience; it reduces intervention costs, and can even benefit the clinician experience (2, 3). Such empowerment of patients is therefore a welcome and much needed evolution in the healthcare relationship – promoting patients’ self-management, self-efficacy, decision making, shared responsibility for health outcome, and increased capacity for patients act on issues that they define as important (2).
Technology is key for accelerating this evolution, from providing information, to gathering data, and triggering timely personalised healthcare intervention, the impact of technology on patient empowerment and shared decision making is everywhere.
Patient empowerment and technology
Scientific and technological innovations have been proven to play a very notable role in healthcare, not only as an aid or facilitator for diagnosis and treatment, but also in healthcare management, delivery and learning about patient empowerment are the source of healthcare system development and patients’ quality of life (5).
In the development, and implementation of health care, technological products are being used to facilitate communication, access provision, interpretation of data, offering real-time connectivity, and enable collaboration between patients and health professionals. Especially in the case of long-term diseases, which have now been declared a major clinical and public health challenge and the leading cause of death worldwide (6, 7).
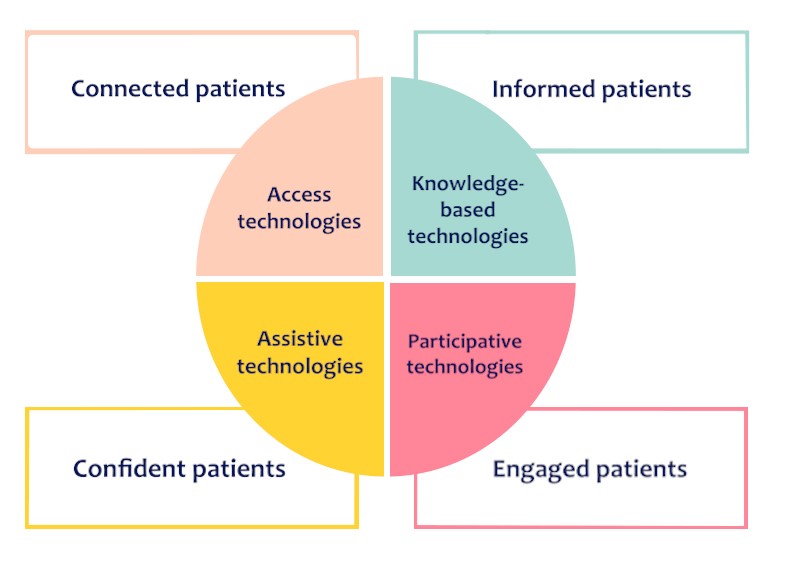
In our review we focus on 4 domains that technologies and digitalization are involved in empowering patients, these are: access technologies, knowledge-based technologies, participative technologies, and assistive technologies.
Access technologies
Access technologies provide a way for patients to remotely and easily access health systems in a timely manner (6).
Health-related apps and software aim to increase the self-management skills of the patient in chronic diseases such as cancer. BNT200 is an example of technological advance comes to help patients when they are diagnosed with cancer, in particular Acute myeloid leukemia (AML). A qualitative study of AML patients showed that patients experience a high level of psychological distress shortly after diagnosis. Such psychosocial distress has a direct impact on the ability of the individual to cope effectively with diagnosis and their time receiving chemotherapy in hospital. BNT200 is a digital therapeutic that designated as a medical device intended to treat the anxiety and depressive symptoms created by the unique psychological stressors specific to adult patients with AML. This software to be used in the inpatient setting during the 4-6 weeks associated with high- intensity chemotherapy (HIC) treatment (9). The contents are delivered via a mobile device and is synchronized with the unique timings of in-patient HIC therapy, so the right help is given at the right time to reduce psychological impact. Even though this is used within the hospital setting, BNT200 is a great example of technology improving self-monitoring, ability to identify stress symptoms, and patient self-driven relaxation assignments as well as treatment adjustments to clinical outcomes and quality of life (8).
Knowledge-based technologies
Knowledge-based technology is becoming increasingly essential for providing patients the latest information about their conditions and how to be more active in their treatment process and self-management. By understanding their health condition and needs patients can describe these quicker and more accurately to healthcare workers during a consultation, even proactively gathering relevant data for treatment decisions.
- Patient education helps patients and their families to have a better understanding of the relevance, potential impact, and how to act on medical advice. Online communities such as online patients’ portals are being enhanced to provide a library of medical education including relevant disease information, self-management strategies, journal entry points for at home recording of relevant information, access to up-to-date personal test results, and secure e-mail/messaging systems that allows patients to ask questions.
In addition, when used in a patient-doctor partnership, accessing to patients’ portals gives patients the information and means to be able to complement health care expertise and accurately translate recommendations and instructions into daily self-care strategies. This in-practice use can expand patients’ knowledge about health conditions and treatments while also helping them find emotional and social support from healthcare when needed (10, 11).
Education delivered at the right time and in an accessible way matters. A recent meta-analysis of 320 articles about patient information found that education was the most successful at improving physiological progress and health outcomes out of all experimental effects (10).
- Lack of patient awareness about their conditions has been identified as the most common barrier to active self-management of chronic diseases. Technology can play a significant role in tackling this issue. Intelligent Diabetes Management (IDM) has now been around for a few years but remains an excellent example of how technology can support the daily self-care. IDM is a smartphone application for patients with type 1 diabetes developed by the University of Alberta. This application includes a glucose and meal tracker, providing detailed records in daily basis. The Data can be viewed on the IDM website and formatted to present insulin dose, planned physical activity, carbohydrate intake, hypoglycemia, etc. This application also provides the median values of blood glucose from meal to meal and overnight. so helps patients to make adjustments in insulin dose in a convenient and user-friendly manner (10, 8). This is one of many applications, the majority of which positively effect patient outcomes, including control of blood glucose levels and hypoglycemia rates (8). This is only the start, introducing artificial intelligence into the systems is promising even greater aid for diabetes Type 1 or 2 patients when self-managing (4).
Participative technologies
Patients’ values and goals of healthcare should be considered as an important part of patients’ treatment and health outcome aims. Participative technologies can pave the way by encouraging and enabling patients to be more actively involved in managing their own health. The use of technology to enhance interactive and two-way sharing of data between patients at home and healthcare professionals is causing a paradigm shift with the patient’s voice joining their doctors in the centre of their care (6 , 12).
Here technology offers a better usage of resources by making participation more efficient and providing patients greater opportunity to discuss options with their family and friends about complex treatment demands and possible consequences (12).
Participative technology and shared decision-making tools, empower patients to be clearer when identifying and communicating their needs, values, goals and decisions with their healthcare delivery team. In the process, the clinician shares information about the health condition, their recommended management options, and the possible outcomes. Together, they reach and implement a decision informed by the best evidence and patients’ preferences to truly personalize the therapy that is implemented. Technological advance means that this level of interaction is accessible for more people through the use video-communication, web-based aids, smartphone applications, and digital booklets that make the dialogue easier and more timely (5, 12_15) .
For instant, during the COVID-19 pandemic many people had to make decisions about vaccination whilst being pummeled by overwhelming wave of conflicting opinions and ideas circulating in the media. It was challenging. At least nine main decision aids were developed that covered choices related to covid-19 vaccination. These could be supported by the hospitals and local healthcare providers to help people reach their own informed choice in a way that healthcare providers – restricted to a clinic visit schedule – couldn’t for the whole population in their care. The Hospital of Ottawa’s international is an example of an institution who did this. The digital decision aids provided cover vaccination decisions for the general population as well as for people with rheumatologic diseases, and people who are pregnant or breastfeeding. This is an example of developers tackling vaccine hesitancy through shared decision making and using research to support their approach. IPDAS criteria (International Decision Aid Standards), a literature review, and qualitative interviews with patients were conducted to fully understand the drivers and considerations around vaccine hesitancy in the population. A group of clinicians and patients was then assembled to use these data and co-create the decision aid, before testing it and then releasing for general benefit (14).
Assistive technologies
Assistive technologies provide greater independence by enabling a patient to perform tasks outside practitioner’s intervention. These directly benefit patients because successful self-management of a chronic disease allows people to live their life independently despite their medical conditions, to feel healthy, and most importantly – to not feel like a patient even though they may manage an ongoing challenge (16).
These kinds of technologies cover a wide range of tools such as memory aids, reminder messages, medication aids, clocks, calendars and sensors around the home to detect situations that can be potential hazards (17). A great example is again from diabetes management – a technology called “Continuous glucose monitoring (CGM)”. This is a device that perform real-time CGM (rtCGM), provide near-continuous data so that patients can see how their blood glucose has changed, and alarms to alert the user of rapid glucose increases or drops. With improvements in the algorithms (discussed earlier) the accuracy of these is improving all the time – helping people manage their condition as well as having fewer alerts or worries about a crash when they’re sleeping. Insulin infusion suspension for pumps can also be linked into the system to help with managed administration. When sensor, algorithm and pump are combined for patients’ self-management improvements in blood glucose and a reduction in hypoglycemia incidences by up to 72% in people with type 1 diabetes (16).
To have enough information to act and evaluate achievements every day is empowerment. Most diabetes patients felt safer and more in control when using CGM devices because they could see glucose readings in real-time almost effortlessly (16).
Conclusion
For empowerment to happen people need better access to resources and information: offering patients an overview of knowledge related to their conditions and treatment, giving patients the means to join shared-decision making and clearly communicate what is helpful for them and according to their needs, and then providing systems that help people to have more control over their life and be more independent. Time and again empowering patients has helped to improve their health. Many patients can self-manage conditions well and relieve some of the stress in primary and secondary healthcare, but only if they have the information, decisional power, and tools to do so. This way technology can pave the way for healthcare providers and patients help each other.
References:
- Yvonne Bombard, G. Ross Baker, Elaina Orlando, Carol Fancott, Pooja Bhatia, Selina Casalino, et al. Engaging patients to improve quality of care: a systematic review. Implementation Sci 13; 2018
- Risling T, Martinez J, Young J, Thorp-Froslie N. Evaluating Patient Empowerment in Association With eHealth Technology: Scoping Review. J Med Internet Res; 2017
- Martin Gellerstedt, Jeanette Melin, Victoria Johansson, Eva Angenete. Are patients willing to take a more active role? Questionnaires to measure patients’ willingness to be empowered. Patient Education and Counseling: Volume 105, Issue 3; 2022.
- Artificial Intelligence Offers Significant Rate of Remission for Type 2 Diabetes Compared to Standard Care; June 2022, Available from: https://diabetes.org/newsroom/press-releases/2022/artificial-intelligence-offers-significant-rate-remission-type-2-diabetes-compared-to-standard-care
- Luchen Pan, Xiaoru Wu, Ying Lu, Hanqing Zhang, Yaoling Zhou, Xue Liu, Shenglin Liu, et al. Artificial intelligence empowered digital health technologies in cancer survivorship care: A scoping review. Asia-Pacific Journal of Oncology Nursing. Volume 9, Issue 12; 2022.
- Akeel AU, Mundy D. Re-thinking technology and its growing role in enabling patient empowerment. Health Informatics J; 2019.
- Inger Ekman and others, Person-Centered Care — Ready for Prime Time, European Journal of Cardiovascular Nursing, Volume 10, Issue 4, 1 December 2011, Pages 248–251.
- Nathan A. Boucher, Kimberly S. Johnson, Thomas W. LeBlanc. Acute Leukemia Patients’ Needs: Qualitative Findings and Opportunities for Early Palliative Care. Journal of Pain and Symptom Management, Volume 55, Issue 2, 2018, Pages 433-439.
- Blue Note Therapeutics Receives Breakthrough Device Designation for Prescription-only Digital Therapeutic for Acute Myeloid Leukemia; January 2022, Available from: https://bluenotetherapeutics.com/news/blue-note-therapeutics-receives-breakthrough-device-designation-for-prescription-only-digital-therapeutic-for-acute-myeloid-leukemia/
- Imon Chakraborty, Sisira Edirippulige, P. Vigneswara Ilavarasan, The role of telehealth startups in healthcare service delivery: A systematic review, International Journal of Medical Informatics, Volume 174, 2023.
- Lau M, Campbell H, Tang T, Thompson DJ, Elliott T. Impact of patient use of an online patient portal on diabetes outcomes. Can J Diabetes; 2014.
- Alami H, Gagnon M, Fortin J. Involving Citizen-Patients in the Development of Telehealth Services: Qualitative Study of Experts’ and Citizen-Patients’ Perspectives. J Particip Med; 2018.
- Fanio J, Zeng E, Wang B, Slotwiner DJ, Reading Turchioe M. Designing for patient decision-making: Design challenges generated by patients with atrial fibrillation during evaluation of a decision aid prototype. Front Digit Health; 2023.
- Barry M J, Härter M, Househ M, Steffensen K D, Stacey D. What can we learn from rapidly developed patient decision aids produced during the covid-19 pandemic. BMJ journal; 2022.
- Clemensen Jane. Patient Empowerment and New Citizen Roles through Telehealth Technologies – The early stage; 2011.
- Alcántara-Aragón V. Improving patient self-care using diabetes technologies. Ther Adv Endocrinol Metab;2019.
- Joseph Sirintrapun and Ana Maria Lopez. Telemedicine in Cancer Care. American Society of Clinical Oncology Educational Book; 2018.



